As countries worldwide work to combat the HIV epidemic, the diagnosis, treatment, and management of HIV continue to present significant challenges. These challenges are even more substantial in the management of pediatric HIV due to the increased complexity of protocols that require well-trained staff, equipped with explicit guidance, to inform accurate decision-making.
In Zambia, gaps in pediatric HIV care are well documented and include failures to:
-
complete serial testing of exposed infants,
-
diagnose infected children,
-
maintain full viral suppression among children on antiretroviral therapy (ART), and
-
successfully transition adolescents to responsible self-care.
Frequently changing clinical responsibilities and national treatment guidelines further complicate pediatric HIV management, as healthcare workers are limited in number and often lack the skills, training, and support to confidently follow updated treatment guidelines. These challenges impact the quality of the treatment and management of pediatric HIV services Zambian health workers are able to provide.
Clinical decision support systems (CDSS) offer an opportunity for clinicians to be better supported in making decisions that are patient-specific while also adhering to standardized treatment guidelines, improving the quality of care and supporting both clinicians and policy makers within the health system with data for informed decision-making.
Decision-supported Electronic Pediatric HIV Intelligent Care (or ‘DelphiCare’)
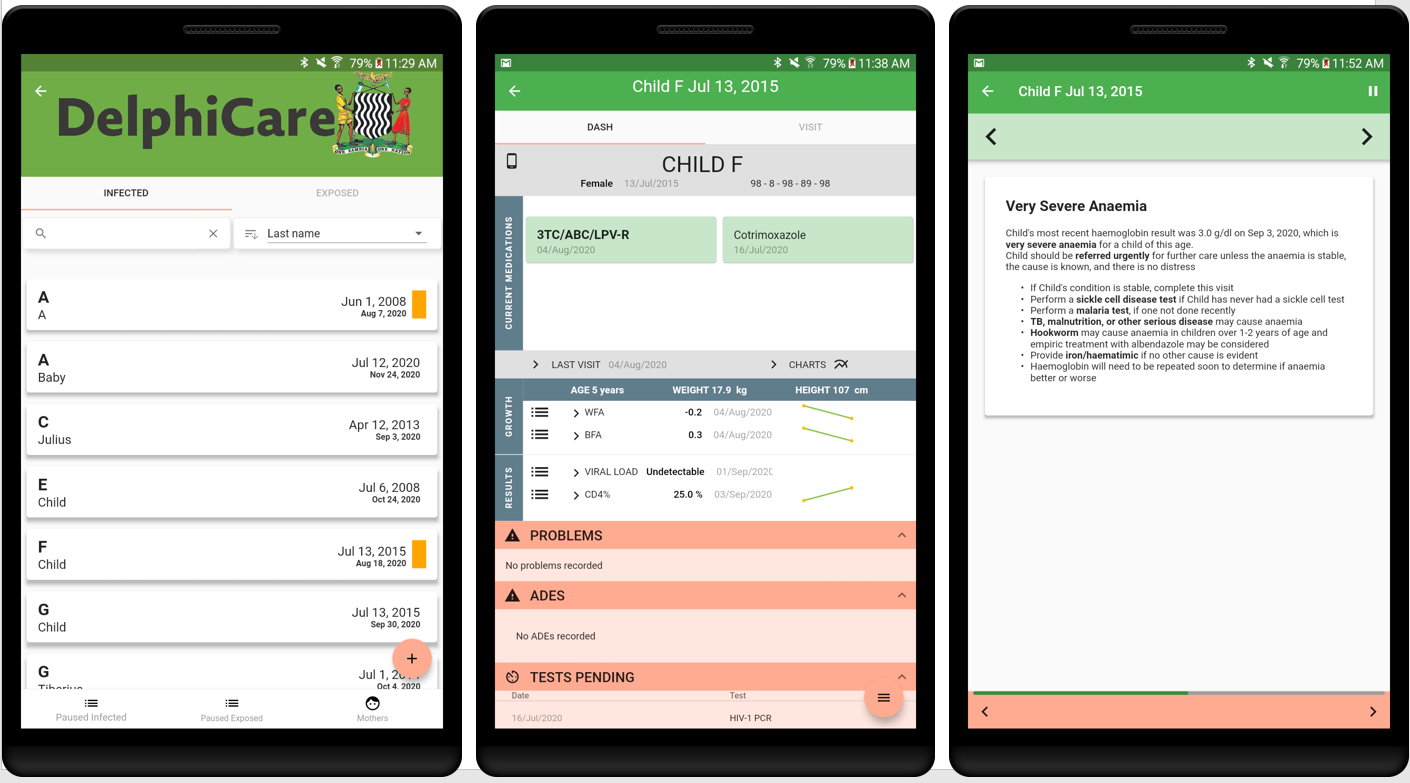
DelphiCare is a CDSS that enables healthcare workers at facilities in Zambia to provide longitudinal, expert-level management of HIV-exposed infants and HIV-infected children. A shift from paper-based pediatric HIV care that loosely follows national guidelines to care guided by a CDSS represents a transformative system change capable of reducing the number of new HIV infections, increasing coverage of quality health services, and strengthening the capacity of facilities and countries to control HIV disease in children.
Addressing all aspects of care, DelphiCare provides recommendations and tailored counseling messages to help providers offer appropriate treatment and support families in promoting adherence. DelphiCare is based on an Android tablet and walks the clinician through each step of care delivery in comprehensive, tailored visits for each child, and alerts the clinician when the child is late for a visit or lost to follow-up. The system creates a personalized dashboard for each child, indicating pending and recent test results, current treatment and adverse drug events, and graphs growth and key test result trends over time.
The DelphiCare system focuses on the following areas:
-
monitoring the breastfeeding mother,
-
testing family members,
-
offering counseling messages on infant feeding and adherence,
-
screening for illness,
-
ordering and interpreting tests,
-
treating HIV and TB,
-
addressing psychosocial barriers such as disclosure of diagnosis, and
-
recommending follow-up.
“[With DelphiCare,] we have something to use as point of care for children in [Maternal and Child Health] without referring to hard copy guidelines always.” —Allidah Njovu, Maternal-Child Health Nurse, Pemba Clinic, Pemba, Zambia
In designing the DelphiCare system, we adhered to several important principles of clinician-led and patient-oriented development:
-
Clinical content written by clinicians themselves in a no-code environment to capture the many nuances in complex clinical logic and intuitively align with the flow of good care. We used Logiak software, enabling clinicians to write and validate logic without coding, eliminating the gap between clinician and developer.
-
Alignment with national guidelines to reflect country-specific guidance and rapidly updating and remotely re-deploying the system to reflect updates without delay.
-
Consultations with and testing by local pediatric HIV experts to ensure that the app’s logic, medication and test recommendations, and counseling messages are not only correct, but are also relevant to the context.
-
Reflections from users through user-centered design, testing, and optional feedback after every patient encounter to ensure the system is designed for the user, is easy to use, addresses identified needs, and rapidly identifies and resolves issues.
-
Small group, on-the-job training conducted by an experienced clinician-educator to create a safe space to learn, ask questions, practice, and receive supportive supervision in the initial patient interactions.
-
Regular monitoring of user activity and program data to spot anomalies that might indicate user misunderstanding, a potential system error, and/or an opportunity for creating a more intuitive user interface.
“Now we have a tool that will give us a reason as to why a child seroconverted [produced detectable levels of HIV antibodies]. It also is helping us to track the mother’s adherence to treatment.” —Tonga Machenje, Clinical Officer Shampande Clinic, Choma, Zambia
Initial results and the potential for the future
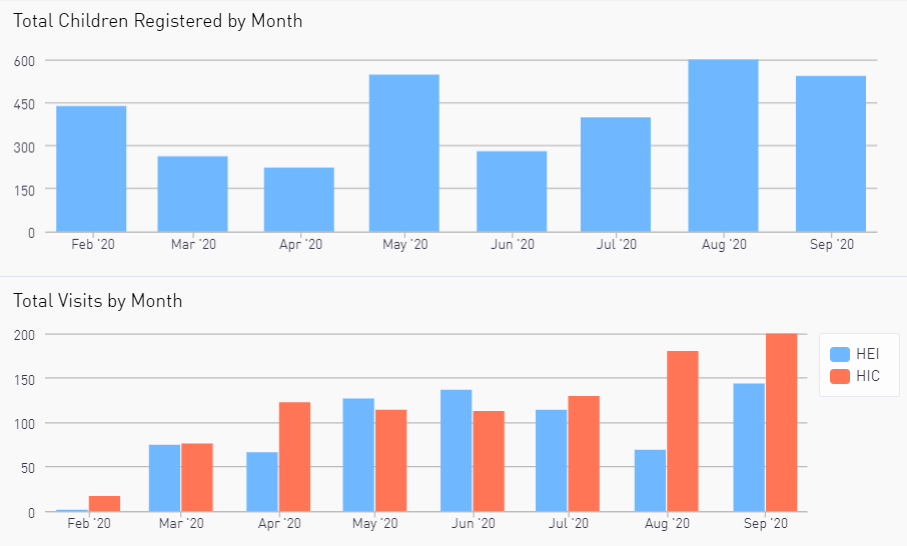
The DelphiCare system was piloted in Zambia from February-September 2020. The system was operational in 11 sites within 4 districts in Southern Province, with over 3,350 children registered. Initial results are promising:
-
DelphiCare identified 1 out of 8 HIV-exposed children to be at high risk of HIV acquisition and implemented prophylactic measures.
-
In over 1/3 of HIV-infected children, DelphiCare identified a sub-optimal regimen and recommended a change in antiretroviral therapy (ART).
-
Among HIV-infected children who started ART, 100% were initiated on the recommended ART regimen according to Zambian guidelines.
-
In 1 out of 6 visits, DelphiCare provided a recommendation not known to the healthcare worker.
-
Short time commitment: A DelphiCare visit for HIV-exposed infant and HIV-infected child visits took an average of approximately 3 and 8 minutes, respectively. Remote feedback showed that most clinicians (96%) said a visit with DelphiCare was either faster than or the same amount of time as a regular visit.
The successes of DelphiCare provide evidence that a CDSS that comprehensively addresses factors affecting the outcome of a complex chronic condition is not only possible, but has the potential to significantly improve health outcomes by providing clinical decision support for healthcare providers, coordinating care among these providers, and facilitating a more patient-centered care. Such a system holds promise for the management of pediatric HIV as well as other complex chronic diseases that require lifetime management; in short, it shows that clinician decision support systems are an opportunity to significantly bolster care delivery, improve quality of life, and save lives.



